NURS-FPX6011 Assessment 2 Traumatic Brain Injury Care Report Example
NURS-FPX6011 Assessment 2 Traumatic Brain Injury Care Report Example
Traumatic Brain Injury Sample Paper
Introduction
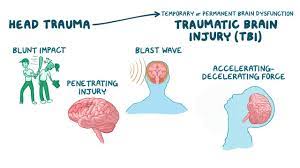
Traumatic Brain Injury (TBI) is defined as an injury that affects the general functioning of the brain. According to the Center for Disease Control and Prevention (CDC) (2022), traumatic brain injuries as some of the leading causes of death, morbidity, and disability in the United States. An estimated 176 people died each day from complications related to TBI in the year 2020, with more than 200,000 hospitalizations in the year 2019 being attributed to complications related to traumatic brain injuries (CDC, 2022).
Motor vehicle accidents, falls, sports-related injuries, and abuse are some of the major causes of traumatic brain injury. The incidence of TBI has been found to be more prevalent in males than females. Extremes of age are also related to increased incidence of the condition, with most patients being people above the age of 65 (CDC, 2022). This essay highlights improvement strategies to improve outcomes related to traumatic brain injury.
The Outcome of the Health Improvement Initiative
Traumatic Brain Injury is attributed to great lapses in memory and the overall cognitive processes. This impact was extensively observed especially among the elderly. Improvement strategies that were observed to greatly improve results in TBI include exercise, meditation, and therapy. Research by Safe Headspace involving almost 400 individuals aged between 40 to 80 years showed significant improvements in overall functioning following traumatic brain injury (Capella University, n.d.).
Short to medium-term memory improved by 61% in 75 out of the 400 individuals who consistently engaged in aerobic exercises for a consistent period of four months (Capella University, n.d.). A 15% improvement in muscle control and a 25% in overall mood was also noted over the same period (Capella University, n.d.). Of the 21 individuals engaging in meditation, improvement in both mood and memory was reported at 70%, with a 32% increase in muscle control (Capella University, n.d.). Therapy in association with medication use improved mood and memory by 26% and 9%, respectively, in individuals undertaking the study (Capella University. N.d.).
Little to no significant outcomes were achieved with other interventions such as puzzle-solving and strength training to enhance memory, and they were, thus, categorized as unsuccessful. This conclusion, however, did not provide a very clear picture since the study lacked a control group, and it was therefore not possible to clearly define the outcome of the interventions among patients suffering from either PTSD or TBI. The research indicated that exercise, meditation, and therapy are vital in improving results secondary to traumatic brain injury.
Strategies for Improving Outcomes
One of the key strategies that can be employed in improving population health outcomes is the segmentation of patient populations. Categorizing patients based on their age, gender, and other characteristics is essential in identifying risk factors that predispose patients to traumatic brain injury (Galgano et al., 2017). Modifying health improvement initiatives based on these categories is also critical in improving health outcomes.
Exercise, therapy, and meditation can be modified based on the patients’ ages, gender, and other factors to ensure optimization and achievement of the best possible results in terms of improving the state of patients following traumatic brain injury. Burnout of nurses may be associated with the categorization of patients. Many patients may be allocated to a small number of nurses specialized in a particular area forcing the nursing staff to work longer durations, consequently leading to burnout.
Identifying risk factors is another important factor in improving health outcomes. In the case of traumatic brain injury, factors such as extremes of age and other underlying conditions such as epilepsy may increase the likelihood of developing traumatic brain injury (Galgano et al., 2017). In instances such as extremes of age, modification of residences and the immediate environment is vital in enhancing safety and consequently minimizing the occurrence of TBI.
Encouraging the use of protective gear after identifying sports as another risk factor is critical in minimizing the risk of developing the condition. Identifying risk factors early allows modification aimed at minimizing or eliminating the occurrence of the condition, in this case, traumatic brain injury. Early identification of risk factors may mean that most nursing practitioners will spend the majority of the time screening and addressing risk factors, minimizing time spent on patients’ actual care, significantly impacting their overall well-being.
The utilization of primary medical care models is another critical strategy for the improvement of health outcomes. Primary medical care focuses on patient-centered care that is comprehensive, well-coordinated, and team-oriented, with the overall aim of improving both the quality and safety of care (Herrmann, 2021). This delivery method is important in ensuring the patient’s overall wellness while also preventing complications related to the condition.
In this scenario, using this model, the health care professional will focus on optimizing the strategies to improve patient outcomes to ensure the overall improvement of the patient’s status following traumatic brain injury. The primary care model is faced with the challenge of lack of choices since each health care practitioner has a particular way they work with patients in promoting their health, tending to be more compatible with some patients than others.
Individualized Personal Care Approach.
Individualized patient care is important as it considers the patient’s preferences and other factors during health care administration. Understanding and addressing the patient’s primary concern is important in offering individualized care. In the case of TBI, patients may be worried about memory loss. Engaging the patient in exercises, meditation, and other activities that improve the patient’s memory is vital. Where muscle movement is the main issue, modified aerobic exercises aimed at improving the patient’s overall state can be initiated.
Education of the patient regarding the condition and the choice of treatment is important in enabling the patient to better understand his or her condition. The overall aim of the individualized personal care approach is to ensure improved quality of care administered and consequently improve patient satisfaction while also enhancing awareness and understanding of the condition.
The care of Mr. Nowak will incorporate both exercise and meditation as they have been shown to have improved results when it comes to improving memory, muscle movement, and mood following TBI. The assumption is that Mr. Nowak will be well following strict adherence to the guidelines provided by the health care professional.
Value and Relevance of Evidence.
Evidence and research are critical in the administration of care. It ensures the provision of the best available and most effective care to improve patient outcomes and satisfaction. Evidence-based practice incorporates the best available evidence, clinical expertise, critical decision-making, patient values, and circumstances, among other factors, to improve care administered. Integrating evidence in personal care translates to improved quality of life. In addition, there is an improvement in the quality and duration of life conferred by the interventions indicated.
The patient expects to receive the most effective care based on the newest, most relevant, and acceptable scientific evidence. Therefore, inculcating evidence in care administration improves patients’ confidence in healthcare professionals. To the health care professional, the evidence provides an avenue to assess the risks and advantages of various procedures (McKinney et al., 2019). This facilitates careful and guided collaboration between care providers and patients in ensuring that the most effective care is administered. Research indicated that meditation and exercise play a major part in helping patients after TBI. This information has guided the individualized care plan formulated for Mr. Nowak.
Evaluation of Desired Outcomes.
Formulation of evaluation questions is the first step in evaluating desired outcomes. The questions should be designed in line with a proper understanding of the idea triggering the intervention, challenges faced during implementation, and knowledge of the available data in assessing outcomes. Patient engagement in formulating the questions is important and recommended as it enables a platform that better understands the outcomes that matter most to them. Evaluation questions are helpful, but they may be subjective, time-consuming, costly, and pose a challenge during analysis and interpretation.
Randomized-control designs are also vital components that can be used to assess desired outcomes. These designs entail the random selection of patients to receive either controlled management or interventions. Observational studies are alternative solutions that may be employed to assess outcomes. These studies facilitate comparison between variations in population and exposure to interventions. These methods are critical in assessing desired outcomes and whether they have been achieved or not. Randomized control designs are helpful. However, they may require multiple sites to render them valid, making them difficult o manage. Loss of relevance emanating from extended trial run times may also be experienced.
Conclusion.
Traumatic brain injury is defined as an injury to the brain that generally affects general functioning. It is a major cause of both mortality and disability. Exercise, meditation, and therapy have been indicated as interventions that significantly improve patients’ overall state following TBI. Basing personal care on evidence is essential as it ensures the administration of the most effective care in ensuring effective outcomes, improved patient outcomes, and satisfaction.
References
Capella University. (n.d.). Evidence-based health evaluation and application [Transcript]. Retrieved from http://media.capella.edu/CourseMedia/MSN6011/evidenceBasedHealthEvaluation/media.asp
Centers for Disease Control and Prevention. (2022, March 21). Get the facts about TBI. Centers for Disease Control and Prevention. Retrieved April 23, 2022, from https://www.cdc.gov/traumaticbraininjury/get_the_facts.html#:~:text=TBI%20is%20a%20major%20cause%20of%20death%20and%20disability&text=There%20were%20over%2064%2C000%20TBI,the%20United%20States%20in%202020.&text=That’s%20about%20176%20TBI%2Drelated%20deaths%20every%20day.
Galgano, M., Toshkezi, G., Qiu, X., Russell, T., Chin, L., & Zhao, L. R. (2017). Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplantation, 26(7), 1118–1130. https://doi.org/10.1177/0963689717714102
Herrmann W. J. (2021). Herausforderungen medizinischer Versorgung im urbanen Raum : Ein Rahmenkonzept zur Primärversorgung in der Stadt [Challenges of medical care in urban areas – a conceptual framework for primary care in the city]. MMW Fortschritte der Medizin, 163(Suppl 6), 3–8. https://doi.org/10.1007/s15006-021-0503-6
McKinney, I., DelloStritto, R. A., & Branham, S. (2019). Nurses’ Use of Evidence-Based Practice at Point of Care: A Literature Review. Critical Care Nursing Quarterly, 42(3), 256–264. https://doi.org/10.1097/CNQ.0000000000000266
Weinstein, A. A., Chin, L., Collins, J., Goel, D., Keyser, R. E., & Chan, L. (2017). Effect of Aerobic Exercise Training on Mood in People With Traumatic Brain Injury: A Pilot Study. The Journal Of Head Trauma Rehabilitation, 32(3), E49–E56. https://doi.org/10.1097/HTR.0000000000000253
Assessment 2 Instructions: Traumatic Brain Injury Care Report
Create a patient-centered care report applying the outcomes of the Population Health Improvement Initiative (PHII). Your report will be based on the scenario presented in the Evidence-Based Health Evaluation and Application media piece.
Master’s-level nurses need to be able to think critically about the evidence, outcomes data, and other relevant information they encounter throughout their daily practice. Often the evidence or information that a nurse encounters, researches, or studies is not presented in the exact context of that nurse’s practice. A key skill of the master’s-level nurse is to be able to transfer evidence from the context in which it was presented and apply it to a different context in order to maximize the benefit to patients in that new context.
Scenario
For this assessment, you will base your report on the scenario presented in the Evidence-Based Health Evaluation and Application media piece. Some of the writing you completed and exported from the media piece can constitute your prewriting and inform the development of your final submission. Further, even though the media piece was framed within one type of care setting, you can extrapolate the situation into another care setting that is more relevant to you. You will still be able to apply community outcomes data to an individual patient or case.
Instructions
For this assessment, you will apply the outcomes of the Population Health Improvement Initiative (PHII) to a patient-centered care report. The bullet points below correspond to grading criteria in the scoring guide. Be sure that your report addresses all of the bullets below, at minimum. You may also want to read the Patient-Centered Care Report Scoring Guide and Guiding Questions: Patient-Centered Care Report [DOCX] to better understand how each criterion will be assessed:
-
- Evaluate the outcomes of a population health improvement initiative.
- Propose strategies for improving the outcomes of the population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence.
- Develop an individualized personal care approach that incorporates lessons learned from a population health improvement initiative.
- Justify the value and relevance of evidence used as the basis for your personal care approach to your patient.
- Propose a framework that could be used to evaluate desired outcomes of your approach to personalizing care for your patients and areas that could be applied to similar situations and patients in the future.
- Write content clearly and logically, with correct use of grammar, punctuation, and spelling.
- Integrate relevant sources to support assertions, correctly formatting citations and references using APA style.
Example assessment: You may use the Patient-Centered Care Report Example [DOCX] to give you an idea of what a Proficient or higher rating on the scoring guide would look like.
APA Resources: You may use the APA Style Paper Tutorial [DOCX] and the APA Style Paper Template [DOCX] to ensure your assessment is formatted in appropriate APA style.
Submission Requirements
-
- Length of submission: 4–6 double-spaced, typed pages. Your report should be succinct yet substantive.
- Number of references: Cite a minimum of 3–5 sources of scholarly or professional evidence that support your evaluation, recommendations, and plans.
- APA formatting: Resources and citations are formatted according to APA style.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
-
- Competency 1: Apply evidence-based practice to plan patient-centered care.
-
-
- Develop an individualized personal care approach that incorporates lessons learned from a population health improvement initiative.
- Competency 2: Apply evidence-based practice to design interventions to improve population health.
-
-
-
- Propose strategies for improving the outcomes of a population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence.
- Competency 3: Evaluate outcomes of evidence-based interventions.
-
-
-
- Evaluate the outcomes of a population health improvement initiative.
- Propose a framework that could be used to evaluate desired outcomes of an approach to personalizing care for patients and areas that could be applied to similar situations and patients in the future.
- Competency 4: Evaluate the value and relative weight of available evidence upon which to make a clinical decision.
-
-
-
- Justify the value and relevance of evidence used as the basis for a personal care approach to a patient.
- Competency 5: Synthesize evidence-based practice and academic research to communicate effective solutions.
-
-
-
- Write content clearly and logically, with correct use of grammar, punctuation, and spelling.
- Integrate relevant sources to support assertions, correctly formatting citations and references using APA style.
-
Patient-Centered Care Report Scoring Guide
| CRITERIA | NON-PERFORMANCE | BASIC | PROFICIENT | DISTINGUISHED |
| Evaluate the outcomes of a population health improvement initiative. | Does not describe the outcomes of a population health improvement initiative. | Describes but does not evaluate the outcomes of a population health improvement initiative. | Evaluates the outcomes of a population health improvement initiative. | Evaluates the outcomes of a population health improvement initiative, and identifies knowledge gaps, unknowns, missing information, unanswered questions, or areas of uncertainty (where further information could improve the evaluation). |
| Propose strategies for improving the outcomes of a population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence. | Does not propose strategies for improving the outcomes of a population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence. | Proposes strategies that are not useful for improving the outcomes or ensuring that all outcomes are being addressed, or that strategies are not based on the best available evidence. | Proposes strategies for improving the outcomes of a population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence. | Proposes strategies for improving the outcomes of a population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence. Acknowledges challenges in the proposed strategies. |
| Develop an individualized personal care approach that incorporates lessons learned from a population health improvement initiative. | Does not develop an individualized personal care approach that incorporates lessons learned from a population health improvement initiative. | Develops an individualized personal care approach, but it does not clearly incorporate lessons learned from a population health improvement initiative. | Develops an individualized personal care approach that incorporates lessons learned from a population health improvement initiative. | Develops an individualized personal care approach that incorporates lessons learned from a population health improvement initiative, and identifies assumptions on which the map is based. |
| Justify the value and relevance of evidence used as the basis for a personal care approach to a patient. | Does not justify the value and relevance of evidence used as the basis for a personalized care approach to a patient. | Presents a weak justification of the value and relevance of evidence used as the basis for a personalized care approach to a patient. | Justifies the value and relevance of evidence used as the basis for a personalized care approach to a patient. | Justifies the value and relevance of evidence used as the basis for a personal care approach to a patient, and identifies knowledge gaps, unknowns, missing information, unanswered questions, or areas of uncertainty (where further information could improve the care approach). |
| Propose a framework that could be used to evaluate desired outcomes of an approach to personalizing care for patients and areas that could be applied to similar situations and patients in the future. | Does not propose a framework that could be used to evaluate desired outcomes of an approach to personalizing care for patients and areas that could be applied to similar situations and patients in the future. | Attempts to propose a framework to evaluate the outcomes of a personalized care approach for patients, but proposed criteria are not measurable or not relevant, or proposed areas of improvement are not likely to be transferable to other cases. | Proposes a framework that could be used to evaluate desired outcomes of an approach to personalizing care for patients and areas that could be applied to similar situations and patients in the future. | Proposes a framework that could be used to evaluate desired outcomes of an approach to personalizing care for patients and areas that could be applied to similar situations and patients in the future. Acknowledges limitations of the proposal. |
| Write content clearly and logically, with correct use of grammar, punctuation, and spelling. | Does not write content clearly and logically, with correct use of grammar, punctuation, and spelling. | Content is not consistently clear and logical, or errors in use of grammar, punctuation, or spelling distract from the message. | Writes content clearly and logically, with correct use of grammar, punctuation, and spelling. | Content is clear, logical, and persuasive; grammar, punctuation, and spelling are without errors. |
| Integrate relevant sources to support assertions, correctly formatting citations and references using APA style. | Does not integrate relevant sources to support assertions; does not correctly format citations and references using APA style. | Sources lack relevance or are poorly integrated, or citations or references are incorrectly formatted. | Integrates relevant sources to support assertions, correctly formatting citations and references using APA style. | Integrates relevant sources to support assertions, correctly formatting citations and references using APA style. Citations are free from all errors. |
Evidence–Based Health Evaluation and Application
Introduction
Public health improvement initiatives (PHII) provide invaluable data for patient–centered care, but their research is often conducted in a context different from the needs of any individual patient. Providers must make a conscious effort to apply their findings to specific patients’ care.
In this activity, you will learn about a PHII, and explore its application to a particular patient’s care plan.
Overview
You continue in your role as a nurse at the Uptown Wellness Clinic. You receive an email from the charge nurse, Janie Poole. Click the button to read it.
Good morning!
At last week’s conference I spoke with Alicia Balewa, Director of Safe Headspace. They’re a relatively new nonprofit working on improving outcomes for TBI patients, and I immediately thought of Mr. Nowak. At his last biannual cholesterol screening he mentioned having trouble with his balance. This may be related to his hypertension, but he believes it’s related to the time he was hospitalized many years ago after falling out of a tree, and expressed distress that this might be the beginning of a rapid decline.
Ms. Balewa will be on premises next week, and I’d like to set aside some time for you to talk.
— Janie
Alicia Balewa
Director of Safe Headspace
Overview
Interview Alicia Balewa to find out more about a public health improvement initiative that might apply to Mr. Nowak’s care.
Interview:
I have a patient who might benefit from some of the interventions for TBI and PTSD you recently studied. What populations did your public health improvement initiative study?
My father came home from Vietnam with a kaleidoscope of mental health problems. That was the 1970s, when treatment options for things like PTSD, TBI, and even depression were very different. Since then there has been a lot of investment in treatment and recovery for combat veterans. That’s excellent news for veterans in treatment now, but they’re not looking at my dad, and how his TBI and PTSD have affected him through mid–life and now as a senior. That’s why I started Safe Headspace: to focus on older patients who are years or decades past their trauma, and find ways to help them.
Which treatments showed the strongest improvement?
Exercise. We were able to persuade about half of our participants — that’s around 400 people, mostly men ages 45–80 — to follow the CDC’s recommendations for moderate aerobic exercise. Almost everyone showed improvement in mood, memory, and muscle control after four weeks. After that a lot of participants dropped out, which is disappointing. But of the 75 who stuck with it for another three months, muscle control improved 15%, mood improved 22%, and short–to–medium term memory improved 61%. We didn’t specify what kind of exercise, but we did ask them to record what they did every week, so that data is available.
Second was medication and therapy. Most of our participants didn’t receive any kind of psychotherapy in the years immediately following their trauma, so we had everyone assessed by a team of psychotherapists. As a result of those assessments, 40% of participants started on anti–depressant medication and 9% started taking anti–psychotics. Those who started taking medications now have regular contact with a therapist to manage that care. With some help at home to stick to the regimen, all but a few have successfully followed their treatment plans. They’ve reported a 26% improvement in mood over six months, and a 6% improvement in memory.
The third treatment I want to mention is meditation. We only had a small group interested in trying it, but the results were dramatic. We prescribed daily meditation at home, just 10 to 15 minutes, with a weekly hour–long guided group meditation for all 23 participants. After three weeks we lost two to disinterest, but the other 21 showed improvements of over 70% in mood and memory, and 32% in muscle control.
Have you tried anything that hasn’t worked?
Sure. There are memory exercises for patients in elderly care, and things like Sudoku and crossword puzzles. We didn’t see any gains with those. Some of our participants preferred strength training to aerobic exercise, and the only improvement we saw in that group was in muscle control, but only 4%, which is significantly less than the aerobic group.
I should also say that we were working with a willing group of participants. They knew they needed help, and were motivated to get it. One of the hurdles we see with veterans, especially in older generations, is an unwillingness to acknowledge that they have a problem. We haven’t had to wrestle with that because everyone who volunteers to participate wants to be there.
Your organization is intervening with people who have TBI and PTSD simultaneously. We have a patient with moderate TBI suffered almost 40 years ago, but no history of PTSD. Have you separated your population and studied each separately?
We haven’t, no. In some cases we could, for those who come in with previous diagnoses and medical records. But we have participants who either weren’t diagnosed, were under–diagnosed at the time, or don’t have records to show us.
Conclusion
As you’ve seen, a PHII can apply to a patient under your care. But it’s not always a perfect fit, and it’s important to think carefully about how your patient’s condition, symptoms, background, and experience compare to that of participants in a PHII.
You may find it helpful to download the responses you made in this activity.
Guiding Questions
Patient-Centered Care Report
This document is designed to give you questions to consider and additional guidance to help you successfully complete the Patient-Centered Care Report assessment. You may find it useful to use this document as a pre-writing exercise or as a final check to ensure that you have sufficiently addressed all the grading criteria for this assessment. This document is a resource to help you complete the assessment. Do not turn in this document as your assessment submission.
Evaluate the outcomes of a population health improvement initiative.
- Which desired outcomes did the PHII achieve?
- How have these outcomes positively affected the community’s health?
- How did outcomes vary across demographic groups?
- Which desired outcomes were not achieved by the PHII?
- To what degree did the PHII fall short of achieving these outcomes?
- How did outcomes vary across demographic groups?
- What factors (institutional, community, environmental, resources, communication, et cetera) may have contributed to these outcomes not being achieved?
Propose strategies for improving the outcomes of the population health improvement plan, or ensuring that all outcomes are being addressed, based on the best available evidence.
- For desired outcomes that were not achieved, what strategies or actions could you take to help improve performance?
- In other words, how would you specifically address the factors that may have contributed to the shortfall?
- What evidence (from similar projects, research, or a professional organization resource) supports the strategies or actions you are proposing?
- How does the evidence illustrate the likelihood of improved outcomes if your proposed strategies are enacted?
Develop an individualized personal care approach that incorporates lessons learned from a population health improvement initiative.
- How did the outcomes and lessons learned from the PHII help inform decisions you made in your approach for personalizing care for an individual with a similar health condition to that addressed in the PHII?
- Does your approach to personalizing care for the individual patient address:
- The patient’s individual health needs?
- The patient’s economic and environmental realities?
- The patient’s culture and family considerations?
- Does your approach to personalizing care incorporate the best available evidence (both from the PHII and other relevant sources) to inform the strategies and action you intend to take?
Justify the value and relevance of evidence used as the basis for your personal care approach to your patient.
- Have you noted why the evidence you have presented is valuable and relevant to the patient’s case?
- Have you explained why each particular piece of evidence is appropriate for your chosen patient and their family?
- In other words, have you explained not only how the evidence is appropriate for the health issue you are trying to correct, but also suited to that individual situation of the patient and their family?
Propose a framework that could be used to evaluate desired outcomes of your approach to personalizing care for your patients and areas that could be applied to similar situations and patients in the future.
- Does your framework include criteria that are measurable?
- Are these criteria relevant to your desired outcomes?
- Have you at least noted how the criteria can be used as an evaluative tool?
- Have you noted areas that could be applied to similar situations and patients in the future?
- In other words, which aspects of your approach to the personal care of this patient are most likely to be transferable to other individual cases?
Write content clearly and logically, with correct use of grammar, punctuation, and spelling.
- Is your writing clear and professional?
- Does your writing effectively communicate your evaluation of the PHII and its application to personalized care?
- Is your writing free from errors?
Integrate relevant sources to support assertions, correctly formatting citations and references using APA style.
- Did you use 3–5 sources?
- Are they cited in APA format throughout the plan?
- Have you included an attached reference list? See NURS-FPX6011 Assessment 3 Evidence-Based Population Health Improvement Plan Paper