Capella University NURS FPX 4050 Final Care Coordination Plan Discussion
Capella University NURS FPX 4050 Final Care Coordination Plan Discussion
For this assessment, you will evaluate the preliminary care coordination plan you developed in Assessment 1 using best practices found in the literature.
NOTE: You are required to complete this assessment after Assessment 1 is successfully completed.
Assessment 4 Instructions: Final Care Coordination Plan
For this assessment, you will evaluate the preliminary care coordination plan you developed in Assessment 1 using best practices found in the literature.
NOTE: You are required to complete this assessment after Assessment 1 is successfully completed.
Care coordination is the process of providing a smooth and seamless transition of care as part of the health continuum. Nurses must be aware of community resources, ethical considerations, policy issues, cultural norms, safety, and the physiological needs of patients. Nurses play a key role in providing the necessary knowledge and communication to ensure seamless transitions of care.
They draw upon evidence-based practices to promote health and disease prevention to create a safe environment conducive to improving and maintaining the health of individuals, families, or aggregates within a community. When provided with a plan and the resources to achieve and maintain optimal health, patients benefit from a safe environment conducive to healing and a better quality of life.
This assessment provides an opportunity to research the literature and apply evidence to support what communication, teaching, and learning best practices are needed for a hypothetical patient with a selected health care problem.
20210119145158nurs_fpx4050_murfernandezyailin_assessment1_3
You are encouraged to complete the Vila Health: Cultural Competence activity prior to completing this assessment. Completing course activities before submitting your first attempt has been shown to make the difference between basic and proficient assessment.
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Adapt care based on patient-centered and person-focused factors.
-
- Design patient-centered health interventions and timelines for a selected health care problem.
- Competency 2: Collaborate with patients and family to achieve desired outcomes.
-
- Describe priorities that a care coordinator would establish when discussing the plan with a patient and family member, making changes based upon evidence-based practice.
- Competency 3: Create a satisfying patient experience.
-
- Use the literature on evaluation as a guide to compare learning session content with best practices, including how to align teaching sessions to the Healthy People 2020 document.
- Competency 4: Defend decisions based on the code of ethics for nursing.
-
- Consider ethical decisions in designing patient-centered health interventions.
- Competency 5: Explain how health care policies affect patient-centered care.
-
- Identify relevant health policy implications for the coordination and continuum of care.
- Competency 6: Apply professional, scholarly communication strategies to lead patient-centered care.
-
- Apply APA formatting to in-text citations and references, exhibiting nearly flawless adherence to APA format.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
Preparation
In this assessment, you will evaluate the preliminary care coordination plan you developed in Assessment 1 using best practices found in the literature.
To prepare for your assessment, you will research the literature on your selected health care problem. You will describe the priorities that a care coordinator would establish when discussing the plan with a patient and family members. You will identify changes to the plan based upon EBP and discuss how the plan includes elements of Healthy People 2020.
Note: Remember that you can submit all, or a portion of, your plan to Smarthinking Tutoring for feedback, before you submit the final version for this assessment. If you plan on using this free service, be mindful of the turnaround time of 24–48 hours for receiving feedback.
Instructions
Note: You are required to complete Assessment 1 before this assessment.
For this assessment:
- Build on the preliminary plan, developed in Assessment 1, to complete a comprehensive care coordination plan.
Document Format and Length
Build on the preliminary plan document you created in Assessment 1. Your final plan should be a scholarly APA formatted paper, 5–7 pages in length, not including title page and reference list.
Supporting Evidence
Support your care coordination plan with peer-reviewed articles, course study resources, and Healthy People 2020 resources. Cite at least three credible sources.
Grading Requirements
The requirements, outlined below, correspond to the grading criteria in the Final Care Coordination Plan Scoring Guide, so be sure to address each point. Read the performance-level descriptions for each criterion to see how your work will be assessed.
- Design patient-centered health interventions and timelines for a selected health care problem.
-
- Address three health care issues.
- Design an intervention for each health issue.
- Identify three community resources for each health intervention.
- Consider ethical decisions in designing patient-centered health interventions.
-
- Consider the practical effects of specific decisions.
- Include the ethical questions that generate uncertainty about the decisions you have made.
- Identify relevant health policy implications for the coordination and continuum of care.
-
- Cite specific health policy provisions.
- Describe priorities that a care coordinator would establish when discussing the plan with a patient and family member, making changes based upon evidence-based practice.
-
- Clearly explain the need for changes to the plan.
- Use the literature on evaluation as a guide to compare learning session content with best practices, including how to align teaching sessions to the Healthy People 2020 document.
-
- Use the literature on evaluation as guide to compare learning session content with best practices.
- Align teaching sessions to the Healthy People 2020 document.
- Apply APA formatting to in-text citations and references, exhibiting nearly flawless adherence to APA format.
- Organize content so ideas flow logically with smooth transitions; contains few errors in grammar/punctuation, word choice, and spelling.
Additional Requirements
Before submitting your assessment, proofread your final care coordination plan to minimize errors that could distract readers and make it more difficult for them to focus on the substance of your plan.
Portfolio Prompt: Save your presentation to your ePortfolio. Submissions to the ePortfolio will be part of your final Capstone course.
Final Care Coordination Plan Example
Care coordination is fundamental to the current healthcare system because it entails organizing patient care activities and sharing information among all healthcare stakeholders. The Agency for Healthcare Research and Quality (AHRQ, 2018) presents care coordination as a strategy for meeting patients’ needs and ensuring timely communication. In this sense, it translates to high-quality care delivery, high-value care, and patient satisfaction. Further, coordinated care encourages caregivers to encourage interdisciplinary collaboration and effective communication to prevent diseases and improve patient outcomes.
Since care coordination is a profound concept in bolstering care quality, this final coordination plan borrows insights from assessment one about patients’ preliminary care coordination plan. Therefore, the final plan elaborates on patient-centered interventions for addressing chronic obstructive pulmonary disease (COPD), community resources for improving patients’ well-being, ethical considerations, policy implications, and interventions’ alignment with the Healthy People 2030 framework.
Patient-centered Interventions
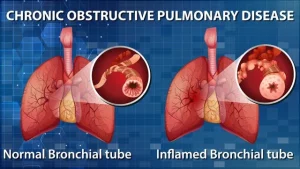
Undoubtedly, chronic obstructive pulmonary disease (COPD) results in various health concerns, including mortalities, morbidity, lengthy hospitalization, increased care cost, and compromised quality of life. According to the Centers for Disease Control and Prevention (CDC, 2021), COPD affects over 16 million Americans, although many vulnerable people are yet to access diagnostics and effective treatment. Globally, over 299 million adults struggle with the disease, leading to increased mortality rates and an upsurging dependency on quality care interventions. As a result, it is essential to consider COPD as one of the leading causes of mortality among chronic conditions.
Before delving into an in-depth conversation regarding the importance of embracing patient-centered and evidence-based interventions for addressing chronic obstructive pulmonary disease, it is essential to focus on its risk factors. The Centers for Disease Control and Prevention (CDC, 2018) identifies smoking, obesity, exposure to environmental or occupational pollutants, family history, and respiratory infections such as pneumonia as the primary risk factors for COPD. Various risk factors for this disease render it multifactorial, prompting healthcare professionals to understand the linkage between causative and contributing aspects before developing individualized treatment and management interventions.
Cigarette Smoking
Cigarette smoking (CS) is an established risk factor for chronic obstructive pulmonary disease because it has multiple effects on the respiratory system. According to Song et al. (2021), active and passive smoking exposes the respiratory tract to harmful ingredients that destroy the structure of the air duct wall, alter the septum of the alveolar wall, and cause interstitial fibrosis. Also, smoking can cause an upsurge in mucous glands’ secretions and obstructive bronchiolitis, aggravating lung tissue lesions. The direct linkage between smoking and COPD enables healthcare professionals to prevent the disease’s prevalence by discouraging the habit.
Exposure to Environmental or Occupational Pollutants
Indoor and outdoor air pollution can increase susceptibility to chronic obstructive pulmonary disease. Lux et al. (2020) argue that airborne chemicals released from industrial processes contain harmful substances, including petrochemicals, polycyclic aromatic hydrocarbons (PAH), formaldehyde, and metals. These pollutants increase respiratory conditions such as asthma and COPD exacerbations. Healthcare professionals can address such risk factors by educating patients about self-protection measures for preventing passive and active exposure to domestic and occupational pollutants.
Obesity
Although debatable, obesity is a risk factor for chronic obstructive pulmonary disease (COPD) because it can worsen the systems of chronic lung diseases. According to the Leader (2020), increased body weight can result in sleep apnea and dyspnea. On the other hand, COPD leads to shortness of breath, respiratory obstructions, and other symptoms such as frequent coughing or wheezing, excess sputum, and trouble taking a deep breath. In this sense, obesity exacerbates COPD symptoms. The linkage between obesity and COPD prompts healthcare professionals to use body mass index (BMI) as an essential factor for assessing, diagnosing, and treating COPD.
Individualized Interventions for Managing COPD
Knowing risk factors for COPD enables healthcare professionals to implement tailored approaches for managing and treating the disease. In this sense, patient-centered care allows caregivers to personalize care delivery mechanisms, promoting shifts from the traditional care delivery systems emphasizing professional-oriented care.
According to the Centers for Disease Control and Prevention (CDC, 2021), it is possible to treat COPD by smoking cessation, avoiding exposure to passive smoke, domestic and occupational pollutants, pulmonary rehabilitation, medication, supplemental oxygen, and observing tenets of healthy lifestyles, including exercise and proper diet plans. Since COPD is a multifactorial condition, it is essential to implement these interventions based on personal factors.
Community Resources
Care coordination emphasizes the importance of collaboration between different entities, departments, and units to ensure quality and timely care. Patients with COPD have many options to consider when accessing community resources for improved care and effective disease management. For instance, they can access information from not-for-profit health organizations, including the Centers for Disease Control and Prevention (CDC), the American Lung Association (ALA), and the National Cancer Institute (NCI). These institutions provide up-to-date self-care information and sponsor campaigns to encourage people to quit smoking and embrace healthy lifestyles. Therefore, they are ideal for patients with COPD.
Ethical Decisions in Designing Patient-Centered Interventions
Undoubtedly, healthcare professionals must incorporate ethical decisions when designing patient-centered interventions for addressing COPD. For instance, the care coordination plan entails tailored approaches for improving the health of patients of diversities, including background, age, worldviews, and socio-economic status. As a result, it is essential to uphold bioethical principles, including beneficence, autonomy, justice, and non-maleficence.
According to Varkey (2020), the four bioethical principles ensure that clinical practices and treatment interventions benefit the patient, avert adverse health effects, safeguard patients’ decision-making roles, and guarantee fairness and equality. It is crucial to ensure patients control schedules and decisions regarding COPD treatment strategies such as physical exercise, pulmonary rehabilitation, diet plans, and self-care education.
Health Policy Implications for Care Coordination and Continuum
The Affordable Care Act (ACA) of 2010 is a landmark policy that affects care coordination and continuum. One of the ACA’s provisions that affect care coordination and continuity when delivering care to patients with COPD is the Hospital Readmissions Reduction Program (HRRP). According to the Centers for Medicare & Medicaid Services (CMS, 2021), the HRRP encourages hospitals to improve communication and care coordination to promote patient engagement and reduce avoidable readmissions.
In this sense, the program authorizes the Centers for Medicare and Medicaid Services (CMS) to penalize health institutions that fail to prevent high readmissions of patients with various conditions, including acute myocardial infarction (AMI), COPD, heart failure (HF), and pneumonia. Eventually, healthcare institutions must coordinate care to avert the likelihood of incurring losses and penalties from Medicare and Medicaid services.
Priorities for Care Coordinators
As a care coordinator, incorporating ethical decisions when designing patient-centered interventions for addressing COPD guarantees patient satisfaction and promotes positive outcomes. In this sense, it is essential to prioritize effective communication, patient engagement and uphold the four bioethical principles when collaborating with patients and family members.
Although the preliminary care coordination plan emphasized the importance of physical exercise, self-care education, progressive nutrition, and social support groups in improving health for patients with COPD, it is essential to establish whether these interventions benefit patients, everts adverse effects of the disease, guarantees equality, and safeguard patient autonomy. The questions regarding thresholds for bioethical principles explain the need to change the care coordination final plan.
Learning Sessions and the Healthy People 2030 Document
Patient satisfaction is vital to care quality because it signifies positive interactions and relationships between caregivers and patients. While familiarizing patients with the preliminary interventions for addressing chronic obstructive pulmonary disease, they expressed the willingness to participate in physical exercise for 30 minutes four times a week and attend education programs to bolster their self-care capabilities. Also, they were comfortable with progressive nutrition education and the plausibility of seeking help from social support groups. Undoubtedly, patient satisfaction was critical in improving care coordination and ensuring the plan’s feasibility.
The Healthy People 2030 framework acknowledges chronic obstructive pulmonary disease as a national issue that requires interdisciplinary collaboration and contingency plans to improve patients’ well-being and ensure positive outcomes. Therefore, it emphasizes various foundational principles, including investing to achieve the full potential for communities’ health and well-being, eliminating health disparities to achieve health equity, ensuring leadership engagement, and setting national goals and objectives to guide evidence-based policies or programs for improving health and well-being (Healthy People 2030, n.d). Notably, the care coordination plan for addressing COPD aligns with the foundational principles of the Healthy People 2030 framework.
Conclusion
The final Care coordination plan presents the importance of embracing patient-centered care when treating COPD. Also, it emphasizes the essence of considering ethical aspects when designing patient-centered interventions. Finally, it elaborates on the affordable care act (ACA) and the Healthy People 2030 framework principles. As a result, it is essential to apply Healthy People 2030 and insights from the Hospital Readmissions Reduction Program (HRRP) to promote care coordination to address COPD. Adherence to bioethical principles is equally fundamental because it guarantees patient satisfaction, eliminates health disparities, and reserves patients’ autonomy to influence care trajectories.
References
Centers for Disease Control and Prevention. (2021, October 20). COPD: Symptoms, diagnosis, and treatment. Accessed 16th February 2022 from https://www.cdc.gov/copd/features/copd-symptoms-diagnosis-treatment.html
Centers for Medicare & Medicaid Services. (2021, January 12). Hospital Readmissions Reduction Program (HRRP). Accessed 16th February 2022 from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HAC-Reduction-Program
Healthy People 2030. (n.d.). Healthy People 2030 Framework. Accessed 16th February 2022 from https://health.gov/healthypeople/about/healthy-people-2030-framework
Leader, D. (2020, March 26). Obesity and COPD: Excess weight can worsen symptoms of this lung disease. Accessed 16th February 2022 from https://www.verywellhealth.com/the-role-obesity-plays-in-copd-914698
Lux, H., Baur, X., Budnik, L. T., Heutelbeck, A., Teixeira, J. P., Neumann, E., Adliene, D., Puišo, J., Lucas, D., Löndahl, J., Damialis, A., Goksel, O., & Orru, H. (2020). Outdoor air pollution from industrial chemicals causing new onset of asthma or COPD: A systematic review protocol. Journal of Occupational Medicine and Toxicology, 15(1). https://doi.org/10.1186/s12995-020-00289-6
Song, Q., Chen, P., & Liu, X.-M. (2021). The role of cigarette smoke-induced pulmonary vascular endothelial cell apoptosis in COPD. Respiratory Research, 22(1). https://doi.org/10.1186/s12931-021-01630-1
Varkey, B. (2020). Principles of clinical ethics and their application to practice. Medical Principles and Practice, 30, 17-28. https://doi.org/10.1159/000509119
Verberne, L. D., Leemrijse, C. J., Swinkels, I. C., van Dijk, C. E., de Bakker, D. H., & Nielen, M. M. (2017). Overweight in patients with chronic obstructive pulmonary disease needs more attention: A cross-sectional study in general practice. NPJ Primary Care Respiratory Medicine, 27(1). https://doi.org/10.1038/s41533-017-0065-3